| Welcome to the programme newsletter | Welcome to the latest edition of Humber Acute Services programme stakeholder newsletter. In it you'll find the latest news and updates about the programme, alongside information about how you can get involved, share your ideas or ask questions.
In the next few issues of our newsletter, we want to highlight some of the developments that are taking place, both in and outside of our hospitals, that contribute to the programme’s vision for the future. Some are national programmes others are local initiatives, but in all cases, we are aligning our work with these wider changes. This issue focuses on Maternity Care. | |
|
Explaining Maternity Care
|
|

|
The vast majority of the care that most women receive during their pregnancy journey takes place outside of a hospital. Women and birthing people are cared for before, after and for some women during birth at home or in local health centres, children's centres and other community facilities by teams of midwives working in partnership with specialist doctors and other healthcare professionals.
Through the Humber Acute Services Programme we are working to design the future shape of maternity services across the Humber, considering how to ensure we continue to provide the best, safest care for women in communities. Much of our work has focused on the elements of care that do take place in our hospitals and working to design the future shape of those services.
The vast majority of the approximately 9000 babies who are born every year in the Humber are born in a hospital maternity unit, other types of facility include midwifery-led units and home births. Some of the different ways in which these services can be provided are described below.
What is an Alongside Midwifery-Led Unit?
An Alongside Midwifery-Led Unit (MLU) is a homely environment co-located within a hospital. This type of unit is suitable for all women and birthing people who are having a straight-forward pregnancy; care is provided by midwives. Alongside MLUs allow close access to doctors, operating theatres and other facilities should they be required.
What is a Standalone Midwifery-Led Unit?
A Standalone Midwifery-Led Unit (MLU) is suitable for women and birthing people who are having a straight-forward pregnancy or have given birth before; care is provided by midwives. This type of unit is away from a hospital and so transfer to a hospital for additional care may be necessary in an emergency situation.
What is an Obstetric-Led Unit?
An Obstetric-Led Unit (OLU), also known as a labour ward is suitable for all women and birthing people. In Obstetric-Led Units care is provided by midwives in partnership with doctors and anaesthetists. This allows access to specialist care should it be required; women and birthing people needing a planned caesarean or epidural, or who have underlying health needs, would be cared for here.
What does Labour, Delivery, Recovery, Postnatal (LDRP) mean and how does it work?
An LDRP model of care comprises labour, delivery, recovery, and postnatal care in a private en-suite room that is designed with the aim of replicating a hotel room. The model allows parents and babies to stay in the same area and have clinical staff come to them, as opposed to moving through ward areas. If a caesarean is required, there is access to a dedicated theatre for this purpose.
The LDRP model allows the benefits of an alongside midwifery-led unit whilst not requiring a seperate building/away from a hospital.
What do the different levels of neonatal care mean?
Neonatal care provides specialist levels of care for newborn babies. There are different levels of provision depending on how much support new babies require.
Transitional care is where a mother and baby are cared for together in cases where the baby needs some additional care. Examples of when this may happen are if they are born early (pre 34 weeks gestation), if the baby has mild jaundice, feeding difficulties, or if they require their blood sugar levels monitoring.
Special Care Baby Units (SCBU) (Level 1) are for babies who do not require intensive care and are born after 32 weeks gestation. They may require monitoring of their heart rate or breathing, receive oxygen, have low body temperatures treated, or receive help with feeding (sometimes by using a tube).
A Local Neonatal Unit (LNU) (Level 2) is for babies who require a higher level of care from 27 weeks gestation. This could be: breathing support given through their windpipe (ventilation), short term intensive care, feeding through their veins (parental nutrition), cooling treatment for babies who have had difficult births or become unwell soon after birth. A level 2 unit also provides level 1 care.
A Neonatal Intensive Care Unit (NICU) (Level 3) is the level of care for babies with the highest need for support. NICU is usually for babies who are born before 27 weeks gestation, or for those who become very unwell after birth. The care received there could be for breathing support including ventilation, or if they need to have surgery.
In 2019/2020, 232 babies received neonatal care at Scunthorpe General Hospital, 289 at Diana Princess of Wales Hospital, Grimsby, and 766 at Hull Royal Infirmary.
|
|
|
|

|
Last year, as we started to develop our models for the future of maternity care, we launched a survey to hear from women and their families about what matters to them in maternity services.
An incredible 1133 people participated and shared their views, through the online survey or coming to one of our focus groups.
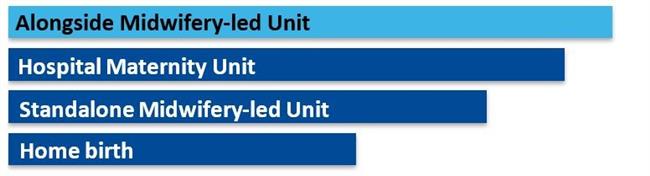
Overall, participants told us that they would prefer to give birth at an Alongside Midwifery Led Unit, as they felt it to be a much safer option with additional support close by if needed.
At Home and at a Standalone Midwifery Led Unit were participants' least preferred locations to give birth at due to concerns around safety should complications arise during labour. The below chart shows how the different options were ranked.
|
|
 |
Overall, women and birthing people told us that being kept safe and well looked after was most important to them when accessing maternity services.
This differs from what other stakeholder groups have told us is most important to them throughout our What Matters to You engagement, with being seen and treated quickly consistently being ranked as most important.
The ‘Your Birthing Choices’ engagement exercise was undertaken to understand what is important to women and birthing people, birthing partners and support people when choosing where to give birth and the feedback gathered has been incredibly important in informing the potential models of care for the future designed through the programme.
We worked with representatives from Maternity Voice’s Partnerships (MVPs) to co-produce our approach to engagement ensuring that it was accessible and inclusive. This included the development of the survey questions, animation video and artwork. The survey was heavily promoted and in total the Your Birthing Choices online promotion reached 310,978 people.
To read the Your Birthing Choices engagement report and the findings please click the banner below.
|
|
 |
| Responding to the Ockenden Review |
|
|
The Ockenden Review
|
The final report of the Independent review of maternity services at Shrewsbury and Telford Hospital NHS Trust (the Ockenden Maternity Review) was published in March 2022. The report was commissioned in the summer of 2017 and has led to a widespread national focus on safety in maternity services.
The report covers four key themes:
- Safe staffing
- Well-trained staff
- Listening to families and learning from incidents
- Avoidable errors and harm to mothers and babies and a failure to learn
Across Humber and North Yorkshire, all hospital trusts and partner organisations are working to ensure services are actively responding to the recommendations in the report and making any changes that are required in the here and now.
For the Humber Acute Services Programme, the publication of the final Ockenden Report represents an important change in the strategic context within which the programme is operating and includes a number of important recommendations when considering the future shape of maternity and neonatal care services across the Humber. These also need to be considered when planning the long term future of maternity services.
Given this important change, we are actively reviewing our proposals against the recommendations and essential actions highlighted within the report to determine which models / variations remain viable.
Specifically, the programme's next steps will be:
- To review the models (and variations) against recommendations from the Ockenden Report to determine viability and any possible workforce implications.
- Re-run workforce modelling/assumptions based on outputs.
- Discount any maternity models that cannot be run safely based on this modelling.
In May, we held a workshop to review and consider the recommendations made within the Ockenden Report against the programme's potential models of care for Maternity and Neonatal services. The purpose of the workshop was to explore how maternity care could be delivered differently and what the advantages and disadvantages would be.
If you have been affected by anything within the Ockenden Report and would like access to advice, guidance or support, please click here to access the Humber and North Yorkshire Local Maternity System website and the 'Ask a Midwife' service.
|
|
|
Can you help?
|
We have been listening to feedback and ideas from people across the Humber over the past 18 months and these have really helped to influence our emerging ideas.
As we develop these ideas for how services could look in the future, we will be continuing to reach out to particular groups within our community, to help us better understand how they may be impacted by any potential changes to acute hospital services. Throughout our work we are seeking to listen to all communities and individuals and reduce health inequalities in the Humber area.
The groups we would particularly like to engage with include:
- People living with serious and enduring mental illness
- People living with poor mental health, including parents and carers.
- Adults and children with learning disabilities or difficulties, including parents and carers.
- People from black, Asian or minority ethnic backgrounds
- People who identify as LGBTQ+
- People affected by homelessness.
How can you help?
- Do you work with or support any of these groups, or know someone who does?
- Do you know of any pre-existing groups we could attend?
- Would you like to be involved and represent the voices of the people you work with?
If you answer 'yes' to any of the above, then please click here to register your interest in hosting or supporting a focus group or other engagement activity over the coming months.
|
|
 |
|
Ask A Question
|
You can ask a question about any aspect of the programme at any time by using the online question portal or by sending an email.
|
|
We launched our revamped Humber Acute Services programme newsletter in July 2021. Each newsletter includes a range of information about the programme and you can access previous editions by clicking the links below:
|
|
|